Download Our Patient Information PDF
Please click here to download our useful information fact sheet »
Subscribe to our e-news
Please click here to subscribe to receive our e-newsletter. Registration is quick and easy »
Contact details
Royal Derby Hospital
Utoxeter road, Derby DE22 3NT
Private sec: 01332785693
NHS Sec: 01332 786773
Private app: 01332 540104
Adhesions
 What are pelvic adhesions?
What are pelvic adhesions?
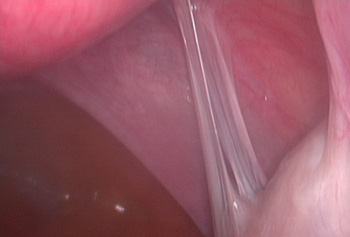
Normally, the genital organs including the womb, tubes and ovaries are lying freely in the pelvis in close proximity but not connected to the bladder or the bowel. All these organs except the ovaries are wrapped in a clear membrane called the peritoneum. Pelvic adhesions are abnormal bands of scar tissue that form in the pelvis and cause organs to stick or bind to one another leading to distortion of the normal pelvic anatomy. Adhesions vary widely in severity and location in the pelvis from few localised bands in one area to extensive thick adhesions involving all the pelvic organs.
What causes pelvic adhesions and how do they form?
There are three well known causes of pelvic adhesions including infection (such as pelvic infection (PID), STD or appendicitis), surgery and endometriosis. In all these conditions, the process of adhesion formation is similar and starts with an inflammation of the peritoneum in response to the surgical trauma or irritation from infection or endometriosis. Fibrous bands of scar tissue form as part of the healing process.
 How common are adhesions?
How common are adhesions?
Adhesion formation is common after any of the three causes mentioned above. The likelihood that adhesions will form after surgery varies in different patients depending on several factors such as the type and extent of surgery, the route of surgery (keyhole or open), the surgical technique used, organs involved, the presence of previous infection, the number of previous surgeries, and the patient’s own predisposition to adhesion formation. The majority of women undergoing open gynaecological surgery will experience some degree of adhesion formation. On the other hand adhesion formation is much less likely after keyhole surgery.
Can adhesions be prevented?
The occurrence of post-operative adhesions cannot be completely eliminated but could be minimised. This could be achieved by performing the surgery laparoscopically whenever possible, delicate handling of tissues to minimise trauma, good control of bleeding (haemostasis) and ample washing with fluid to avoid dryness of tissues. Several adhesion prevention barriers, sprays or fluids have been developed, but none is supported with good evidence. A special fluid called "adept" could be put in the pelvis at the end of the procedure to prevent the organs sticking together during the initial period of inflammation following surgery.
Adhesions can also be minimised by early diagnosis and treatment of pelvic infection and endometriosis.
What symptoms can adhesions cause?
 Although, most pelvic adhesions do not cause problems, they can lead to two main distressing symptoms including pelvic pain and infertility. About 40% of women presenting with chronic pelvic pain are found to have pelvic adhesions. The occurrence of pain in patients with adhesions is due to stretching and pulling of sensitive organs such as the ovaries or bowel during various body movements.
Although, most pelvic adhesions do not cause problems, they can lead to two main distressing symptoms including pelvic pain and infertility. About 40% of women presenting with chronic pelvic pain are found to have pelvic adhesions. The occurrence of pain in patients with adhesions is due to stretching and pulling of sensitive organs such as the ovaries or bowel during various body movements.
Infertility could occur in women with adhesions due to distortion of the delicate relationship between the tube and ovary that is necessary for the passage of the egg from the ovary into the tube. Adhesions around the tube could also make it difficult for the sperms to pass through the tube to reach the egg near its end.
How can adhesions be diagnosed?
Careful assessment of the pattern of pain and laparoscopy (camera inspection of the pelvis) are the key to establishing an accurate diagnosis of pelvic adhesions. Typically the adhesion pain starts shortly after a surgical intervention or an episode of pelvic infection. The pain can either be constant or intermittent, usually sharp in nature and is typically provoked by certain body movements or positions. Some women will experience the pain mainly during intercourse.
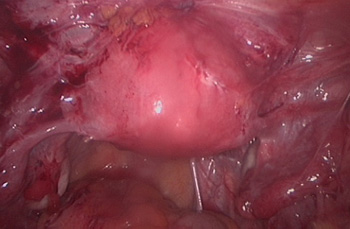 How can adhesions be treated?
How can adhesions be treated?
Pelvic adhesions require treatment only if they are causing symptoms enough to affect the woman's life. The only treatment is surgical removal of the adhesions. A keyhole approach for is the ideal way for this surgery and is superior to the open route as it is associated with less adhesion formation. Only the adhesions that are thought to be the cause of the pain should be removed. Other adhesions away from the area of the pain are better left alone. Patients undergoing surgical removal of adhesions could expect a success rate of about 70%.
